Food Poisoning While Breastfeeding: Expert Advice for Safe Motherhood
Experiencing food poisoning is distressing for anyone, but it raises unique concerns for breastfeeding mothers. You’re not only worried about your own well-being but also the potential impact on your baby. This comprehensive guide provides expert advice on navigating food poisoning while breastfeeding, ensuring the safety and health of both you and your little one. We’ll cover everything from recognizing the symptoms and understanding the risks to effective treatment strategies and preventative measures. Our goal is to empower you with the knowledge you need to make informed decisions and confidently care for your baby during this challenging time.
Understanding Food Poisoning and Its Impact on Breastfeeding
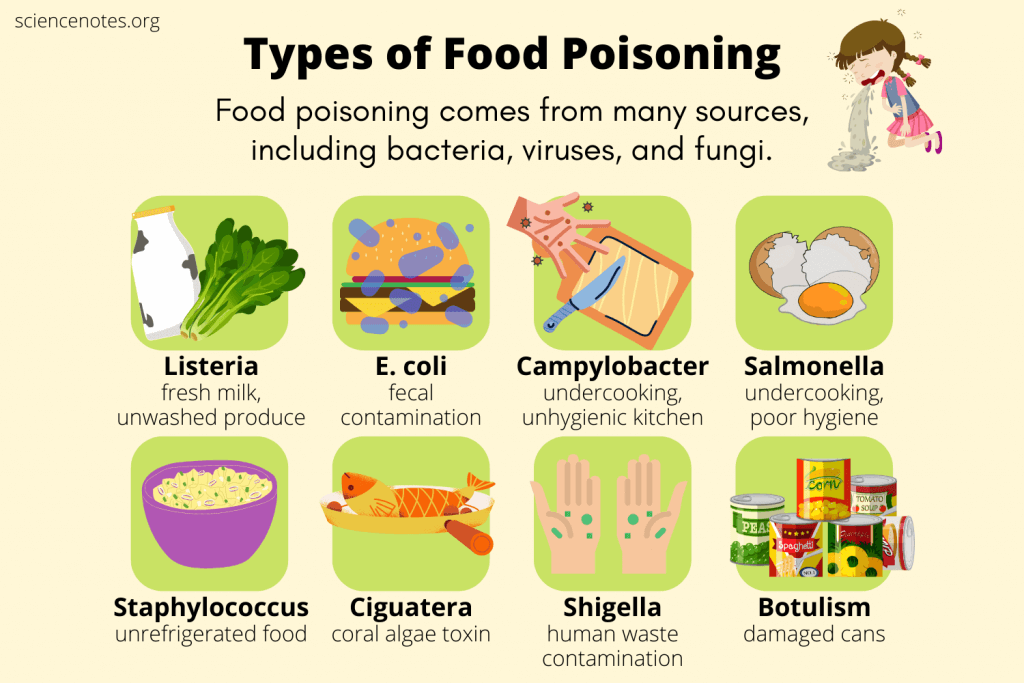
Food poisoning, also known as foodborne illness, occurs when you consume contaminated food or drink. Bacteria, viruses, and parasites are the most common culprits. While the symptoms can range from mild discomfort to severe illness, the primary concern for breastfeeding mothers is whether these pathogens can pass through breast milk to the baby.
Generally, most foodborne illnesses do not directly pass through breast milk. Your body acts as a filter, and the infection typically remains within your digestive system. However, the dehydration and discomfort caused by food poisoning can indirectly affect milk supply and overall well-being, impacting your ability to care for your baby effectively. Understanding this distinction is crucial for managing the situation and making informed decisions about breastfeeding.
Common Causes and Symptoms
Identifying the source and recognizing the symptoms of food poisoning are the first steps toward effective management. Common causes include:
- Bacteria: Salmonella (often found in poultry and eggs), E. coli (often found in undercooked beef and contaminated produce), Listeria (often found in deli meats and soft cheeses).
- Viruses: Norovirus (highly contagious and spread through contaminated food or surfaces), Rotavirus.
- Parasites: Giardia (often found in contaminated water), Cryptosporidium.
Symptoms of food poisoning can vary depending on the specific pathogen involved but often include:
- Nausea
- Vomiting
- Diarrhea
- Stomach cramps
- Fever
- Headache
- Body aches
Symptoms typically appear within a few hours to several days after consuming contaminated food. If you suspect food poisoning, it’s essential to monitor your symptoms and seek medical advice, especially if you’re breastfeeding.
The Role of Hydration and Electrolytes
Dehydration is a significant concern with food poisoning, particularly when experiencing vomiting and diarrhea. Adequate hydration is crucial for maintaining milk supply and overall health. Breast milk is primarily water, so dehydration can directly impact the amount of milk your body produces. Furthermore, the loss of electrolytes through vomiting and diarrhea can lead to fatigue and weakness, making it harder to care for your baby.
Replenishing fluids and electrolytes is a priority. Options include:
- Water: Drink plenty of water throughout the day.
- Oral Rehydration Solutions (ORS): These solutions contain a balanced mix of electrolytes and are specifically designed to combat dehydration.
- Clear Broths: Chicken or vegetable broth can help replenish sodium and other minerals.
- Sports Drinks: While sports drinks can provide electrolytes, they often contain high levels of sugar. Dilute them with water to reduce sugar intake.
Is It Safe to Breastfeed with Food Poisoning?
The good news is that in most cases, it is safe to continue breastfeeding while you have food poisoning. As mentioned earlier, the pathogens causing the illness typically don’t pass through breast milk. Breast milk also contains antibodies that can protect your baby from illness. Continuing to breastfeed provides your baby with these valuable immune-boosting properties.
However, there are situations where caution is warranted. If you’re taking medication to treat food poisoning, it’s essential to consult with your doctor or a lactation consultant to ensure the medication is safe for breastfeeding. Certain medications can pass into breast milk and may not be suitable for infants.
Exceptions and Precautions
While rare, some specific infections can pose a risk to breastfeeding infants. For example, if you have a systemic infection (where the bacteria or virus enters your bloodstream), there’s a slightly higher chance that the pathogen could be present in breast milk. In such cases, your doctor may recommend temporary cessation of breastfeeding or alternative feeding methods.
Other precautions to take include:
- Hygiene: Wash your hands thoroughly with soap and water before breastfeeding or handling your baby. This helps prevent the spread of germs.
- Monitor Your Baby: Watch for any signs of illness in your baby, such as fever, diarrhea, vomiting, or lethargy. If you notice any of these symptoms, contact your pediatrician immediately.
- Stay Hydrated: As mentioned earlier, dehydration can affect milk supply. Make sure you’re drinking plenty of fluids to maintain adequate hydration.
Treatment Strategies for Food Poisoning While Breastfeeding
Treating food poisoning while breastfeeding focuses on managing symptoms, preventing dehydration, and ensuring the safety of your breast milk. Here’s a breakdown of effective treatment strategies:
Home Remedies
For mild cases of food poisoning, home remedies can often provide relief:
- Rest: Get plenty of rest to allow your body to recover.
- Hydration: Drink plenty of fluids, including water, oral rehydration solutions, and clear broths.
- Bland Diet: Start with bland, easily digestible foods like toast, rice, and bananas. Avoid fatty, spicy, or sugary foods, as these can worsen symptoms.
- Ginger: Ginger has anti-nausea properties and can help soothe your stomach. Try ginger tea or ginger ale (in moderation).
- Probiotics: Probiotics can help restore the balance of bacteria in your gut and may shorten the duration of diarrhea.
When to Seek Medical Attention
In some cases, food poisoning can be severe and require medical treatment. Seek medical attention if you experience any of the following:
- High fever (over 101°F or 38.3°C)
- Severe dehydration (signs include decreased urination, dizziness, and dry mouth)
- Bloody diarrhea or vomit
- Severe abdominal pain
- Neurological symptoms (such as blurred vision, muscle weakness, or difficulty speaking)
- If your baby shows signs of illness
Medications and Breastfeeding Safety
If your doctor prescribes medication for food poisoning, it’s crucial to discuss the safety of the medication while breastfeeding. Some common medications used to treat food poisoning include:
- Anti-diarrheal medications: Loperamide (Imodium) is generally considered safe for breastfeeding in limited doses. However, it’s best to consult with your doctor before taking it.
- Anti-nausea medications: Ondansetron (Zofran) is often prescribed for severe nausea and vomiting. It’s generally considered safe for breastfeeding, but discuss the risks and benefits with your doctor.
- Antibiotics: Antibiotics are only necessary for certain types of bacterial food poisoning. If your doctor prescribes antibiotics, make sure to inform them that you’re breastfeeding. They will choose an antibiotic that is safe for your baby.
Always inform your healthcare provider that you are breastfeeding so they can make informed decisions about your treatment plan.
Preventing Food Poisoning: Essential Tips for Breastfeeding Mothers
Prevention is always better than cure. As a breastfeeding mother, you can take several steps to reduce your risk of food poisoning:
- Practice Proper Food Handling:
- Wash your hands thoroughly with soap and water before preparing food.
- Use separate cutting boards for raw meat, poultry, and seafood.
- Cook food to the proper internal temperature. Use a food thermometer to ensure accuracy.
- Refrigerate perishable foods promptly. Don’t leave food at room temperature for more than two hours (or one hour if the temperature is above 90°F).
- Wash fruits and vegetables thoroughly before eating.
- Avoid High-Risk Foods:
- Raw or undercooked meat, poultry, and seafood
- Unpasteurized milk and dairy products
- Raw sprouts
- Deli meats and hot dogs (unless reheated until steaming hot)
- Soft cheeses (such as Brie, feta, and blue cheese)
- Be Careful When Eating Out:
- Choose restaurants with good hygiene ratings.
- Avoid buffets and salad bars where food may have been sitting out for extended periods.
- Order food that is cooked to order and served hot.
- Drink Safe Water:
- Use safe water sources for drinking and cooking.
- If you’re unsure about the safety of your water, boil it for one minute to kill any bacteria or viruses.
Supporting Your Milk Supply During Food Poisoning
Food poisoning can temporarily impact your milk supply due to dehydration and decreased appetite. Here are some strategies to support your milk supply during this time:
- Continue Breastfeeding or Pumping: Even if you’re not feeling well, continue to breastfeed or pump regularly to stimulate milk production. Aim for at least 8-12 feedings or pumping sessions per day.
- Stay Hydrated: Drink plenty of fluids to maintain adequate hydration. This is crucial for milk production.
- Eat Nutritious Foods: Once you can tolerate food, focus on eating nutritious, easily digestible foods. Include plenty of fruits, vegetables, and lean protein.
- Consider Galactagogues: Galactagogues are substances that can help increase milk supply. Examples include fenugreek, blessed thistle, and oatmeal. However, it’s best to consult with a lactation consultant before using galactagogues.
- Rest: Get plenty of rest to allow your body to recover and support milk production.
Expert Insights: Consulting Healthcare Professionals
Navigating food poisoning while breastfeeding can be challenging. Consulting with healthcare professionals can provide valuable guidance and support.
When to Contact Your Doctor
Contact your doctor if you experience any of the severe symptoms mentioned earlier or if you have concerns about your baby’s health. They can assess your condition, provide appropriate treatment, and advise you on the safety of breastfeeding.
The Role of Lactation Consultants
Lactation consultants are healthcare professionals who specialize in breastfeeding. They can provide expert advice on managing milk supply, addressing breastfeeding challenges, and ensuring the safety of medications while breastfeeding. They can also help you develop a personalized plan to support your breastfeeding goals during and after your illness.
Coping with the Emotional Impact of Food Poisoning
Food poisoning can take a toll on your emotional well-being, especially when you’re also caring for a baby. It’s essential to acknowledge and address the emotional impact of this experience.
Managing Stress and Anxiety
Feeling unwell and worrying about your baby can lead to stress and anxiety. Here are some tips for managing these emotions:
- Practice Relaxation Techniques: Deep breathing exercises, meditation, and yoga can help calm your mind and reduce stress.
- Seek Support: Talk to your partner, family members, or friends about your feelings. Sharing your concerns can help you feel less alone.
- Get Enough Rest: Rest is crucial for both physical and emotional recovery.
- Ask for Help: Don’t hesitate to ask for help with childcare or household chores. This will allow you to focus on your recovery.
The Importance of Self-Care
Taking care of yourself is not selfish; it’s essential for your well-being and your ability to care for your baby. Make time for activities that you enjoy and that help you relax. This could include reading a book, taking a bath, or listening to music. Remember, you can’t pour from an empty cup.
Your Well-being Matters: Prioritizing Health During Breastfeeding
Experiencing food poisoning while breastfeeding can be a stressful ordeal. However, by understanding the risks, implementing effective treatment strategies, and prioritizing prevention, you can navigate this challenge with confidence. Remember that in most cases, it is safe to continue breastfeeding, providing your baby with valuable antibodies and immune support. Stay hydrated, monitor your symptoms, and seek medical advice when needed. Most importantly, prioritize your well-being and don’t hesitate to ask for help. By taking care of yourself, you’re also taking care of your baby. Share your questions or concerns about food poisoning while breastfeeding with your healthcare provider to receive personalized guidance and support for a healthy and happy motherhood journey.
